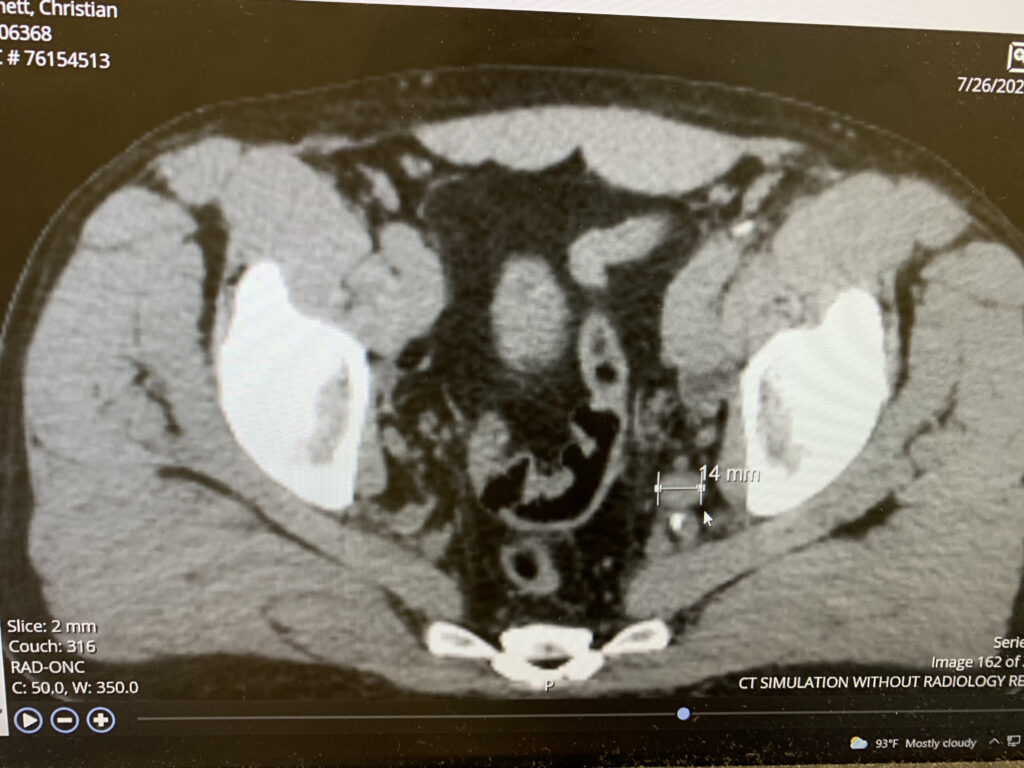
Wednesday 24th February 10.30am: Regular check up with Primary Care Physician. Dr. McGee. I had waited for two months for the appointment on top of waiting for the initial COVID surge to die down. Sunday 7th March: Received results from the check up. My PSA was very high. I was baffled. It was so much higher than the normal range – perhaps they presented it without the decimal point? Monday 8th March: Referral to Dr. Pazona. I got a call from a nurse practitioner at Dr. McGee’s practice that I needed to see a urologist. I was referred to Dr. Pazona. Thursday 11th March 4pm: Appointment with Dr Pazona. He suggested there was a chance of cancer and we had better check. Thursday 18th March 1.30pm: MRI Scan. Friday 19th March 11am: Dr. Pazona told me that the MRI scan was showing prostate cancer probable. Thursday 1st April and Friday 2nd April: Biopsy and unexpected overnight stay in hospital. Prostate cancer was confirmed; an “interesting” form too, called cribriform. So interesting, the hospital wanted to take a specimen for research. It’s not a great one either. As a side note to the story, though the main attraction for a while, as I came around from the general anaesthetic my pulse plummeted to zero, for as long as 90 seconds, and Emily W from the PACU (post anaesthetic care unit) apparently leapt on me, and administered CPR. I came around looking at many doctors and nurses looking down on me to be told that “she’s (Emily) saved your life.” Apparently I, very politely, said “thank you very much.” I was kept in overnight and wore a heart monitor for a month. Nothing much happened. The conclusion of the cardiologist who specialises in the heart’s electrical system was that I had had an extreme vasovagal response. Monday 12th April 8am: CT scan. The scan revealed something suspicious, a lesion, on one of my ribs. If it was bone cancer the 5 year survival rate is less than 30%. With my numbers I had a 10% chance, which is a darn sight higher than the less than 2% chance of getting prostate cancer in the first place. I was scared. The scan report said there were no enlarged lymph nodes in the pelvis, which we know now to be false*. Tuesday 20th April 2.30pm. Second COVID shot, Pfizer. I had side effects: shivers, a headache and I couldn’t sleep, which didn’t help my worries about the bone cancer. It was the worst night of my life. Thursday 22nd April 7am: Bone scan. The technician was SO nice, I was convinced he had seen something. They did a close up of my ribs. I thought “they are scanning my cancer now”. I had an appointment scheduled for the following day. Dr. Pazona, no doubt as relieved as I was, called me within an hour or so of the scan to tell me the lesion was a calcium build up. No bone cancer. Tuesday 4th May 7.45am: Meeting Doctor Daniel Barocas, surgeon. He comes highly recommended. I had also met a radiology oncologist at TriStar, who I didn’t much care for. The system and the protocols drive someone with my numbers to surgery. We had a long chat about the implications of both radiation and surgery. It was clearly pretty serious by now. I didn’t feel there were many sensible options. I elected to have surgery. There was a slot the following Friday. Friday 14th May 5am: Surgery. Using a da Vinci robot, Doctor Barocas removed my prostate (the surgery is called a radical prostatectomy). He said it went very well. I was in the hospital for one night. Home on Saturday. There was considerable abdominal pain, no surprise given the six incisions all around my stomach. I was immobile, had more prescription drugs than a village pharmacy and had a catheter. I couldn’t get into bed as my abdomen was too painful, so I slept on the couch for 4 nights. Monday 24th May 10am: Catheter removed. Removal didn’t hurt (though was weird), but had three incredibly painful spasms, apparently like birthing pains, within the following 24 hours. Drugs were helpful. Wednesday 9th June 5pm: Ultrasound due to scrotal pain. Nothing too worrying. Something to monitor. Not unusual after a radical prostatectomy. Tuesday 15th June 7.45am: Follow up appointment with Doctor Barocas. The pathology report was very positive: No cancer in the margins (at the edges of the prostate), no cancer in the nearest lymph node (that was also removed during the surgery). Feeling good. Friday 18th June 1pm: Hernia concern. After a long drive back from NC, Memorial Day weekend, and after a flight back from MN Wednesday 16th June, the inner thigh of my left leg swelled up. No-one had told me to expect this. Barocas had reported two little hernias after the surgery, and after some googling about hernias, I wondered if the swelling was a hernia. So I went to the Hernia Center. They suggested it was more likely to be a backing up of fluid in the lymphatic system as the system has to get used to having a lymph node removed. They wanted me to return if it swelled up again. Tuesday 22nd June 7.30pm: Trip to the Emergency Room. Left leg swelled up again. Went to Hernia Center but arrived just as they were closing. They sent me to the ER, where I waited for four hours. The doctor who saw me (and the swelling) agreed with the theory of the lymphatic fluid backing up. It’s not unusual and should, over the next year, work itself out. I was told to keep an eye on it. Tuesday 29th June 8am: Survivorship Program Appointment. My six week blood test. Also a pretty depressing meeting about side effects, particularly sexual function. The results of the blood test showed the PSA numbers still too high. This was worrying. I needed a PET scan to see what was going on. Thursday 15th July 2pm: PET Scan. I have a radioactive dye injected into me which will highlight where identifiable cancer is – it can’t show microscopic cells though. It shows I have a cancerous lymph node, a few centimetres from where the prostate was. The cancer had skipped the node that was removed during surgery and gone to this other node deep in my pelvis. Tuesday 20th July 10am: Meeting Dr. Barocas. This was a bad meeting. Probably the worst in the journey. He told me the chances of completely getting rid of the cancer were less than 50%, because the PSA is still high. And if the cancer isn’t killed then there’s a very good chance that it will kill me. He wasn’t sure if it was as low as a 10 or 20% of getting it. That was scary to hear. What’s more, if they don’t get it, he continued, I am young enough to die from it. Older men will generally die of something else because meds can slow down the progression of the cancer, whereas I am young enough to die of it. I asked how many years I have if they don’t get it. He threw out 3,5,7 or 10 years. I wasn’t ready for that! He also laid out the best treatment path; radiation and ADT therapy (Androgen Deprivation Therapy), the latter basically removes any testosterone from my body. The testosterone is essentially the food for the cancer so ADT denies it the nutrition. The side effects though, are not great: loss of bone density, loss of muscle mass, loss of libido, hot flushes/flashes, weight gain, slower metabolism, fatigue, possible depression and mood swings! I could tell it was a difficult meeting for Barocas – he’d actually suggested not having it and me going straight to the radiation doctor. It was also a difficult meeting for me. I was very emotional for a couple of days. Monday 26th July 8.30am, 10am and 5pm: ADT administered (8.30am), meeting Dr. Kirschner (10am), and CT scan to set up for radiation (5pm). I had two heavy loading doses of ADT (Firmagon) injected into my abdomen, which caused considerable pain and then discomfort for a week or so. At 10am, I met Dr. Austin Kirschner. I liked him; academic in style and friendly in tone. He said the chances of getting the rid of the cancer are, for someone like me, generally 50:50, though he thinks for me specifically more like 50-60% because the cancer is very concentrated in that lymph node, though there may be microscopic particles that the PET scan couldn’t detect, and they may have gone beyond the pelvic area. This is a risk but we wouldn’t know about that for about two and a half years because of the ADT. Nevertheless, this was relatively cheery after my meeting with Dr. Barocas a few days prior. Wednesday 4th August 5pm: Therapy. After the last few weeks I feel the need to talk to someone, especially around getting the story straight in my head for why I didn’t find this earlier. I’d been beating myself up and that’s where the therapy would start. This therapist specialises in cancer patients. She was recommended by a friend. It’s been really good. Thursday 5th August 4.30pm: Radiation starts. 39 treatments, one a day every weekday. I choose to have them at end of the day so I can exercise in the morning (to mitigate against the effects of the ADT) and crash out after the radiation if I need to, and I do, at the end of the day. I have to be positioned in EXACTLY the same place everyday – remember, we are dealing in millimetres and I don’t want my bladder or bowel radiated by mistake! Not only do I need to be positioned on the table in the same place every day, but my ‘insides’ need to be in the same place every day…..so an hour before my treatment I have to “evacuate my bowels”, “void my bladder” and drink exactly the same amount of water, and hope that my insides are EXACTLY the same everyday too! The staff are fantastic, full of good humour and hi-tech. It’s like a fling, short-lived, intense and preoccupying. Every day revolves around it and the 4.30 start to the ritual. I park in the same place (too late for the valet parking so I get a slot right outside the door), generally greet the same people and then see (a) whether they are running to time, which is important given that a delay of more than 20 mins is not good with a full bladder and (b) which team of radiologists are working today, so I know how much fun it’ll be. I see Dr. Kirschner every Monday for a check in to see how I am doing – more on that in the next post. The waiting room is the stuff of sad drama and tragedy: generally older men, women of a greater variety of ages, inpatients who get brought down in their beds who, on occasion, look translucent and close to death, and children and teenagers who look baffled, stunned and lost. The TV relentlessly plays the home improvement channel. I got quite used to it over my 39 visits. The treatment doesn’t take long: always a CAT scan to see if I am positioned correctly and then about 5 mins of radiation. Just time for a couple of songs over the treatment room speakers. Friday 3rd September 6am: Jim at the gym. In response to Dr. Kirschner’s advice to focus on resistance training to mitigate the effects of the ADP, Tiffany found Jim at the YMCA in Green Hills. He’s my/our age and good. He has a philosophy – based around failing between 45-90 seconds rather than number of reps – and a laid back manner. Wednesday 29th September 5.30pm: Final treatment. The last few days have been pretty emotional. I’ll write about that in my next post. I’ve said goodbye to the folk not working on Wednesday and already bought flowers and cookies and cupcakes galore. Today is the bell ringing, part of the last day ritual. One of the staff recites a short poem and I ring. I am the only patient around, I have a good group of friends and colleagues who have come to witness the bell ringing, and three of my favourite radiologists. I requested Anita Ward’s “Ring my bell” as the song to accompany the treatment today, to be played loud. The end is both anti climatic in so far as there is no single “event” like the surgery, but in many ways it is way more profound – a unique, terrible, wonderful, crazy, surreal couple of months – each day spending time with some amazing people that I’ll always feel something for.
*Either the cancerous node wasn’t picked up by the scan, or the doctor reviewing the scan didn’t pick it up or the node just hadn’t become enlarged at the time.
This isn’t the end. In some ways it’s just the end of the beginning. I have two years of ADT to go, if I can last that long (apparently only about 50% of people stick it out for the whole two years). After that the body has to readjust to having testosterone again which can take 6-12 months. And only then can they take readings to see if my PSA is up. I had a PSA test on 4th Oct and the score was where it should be: undetectable.